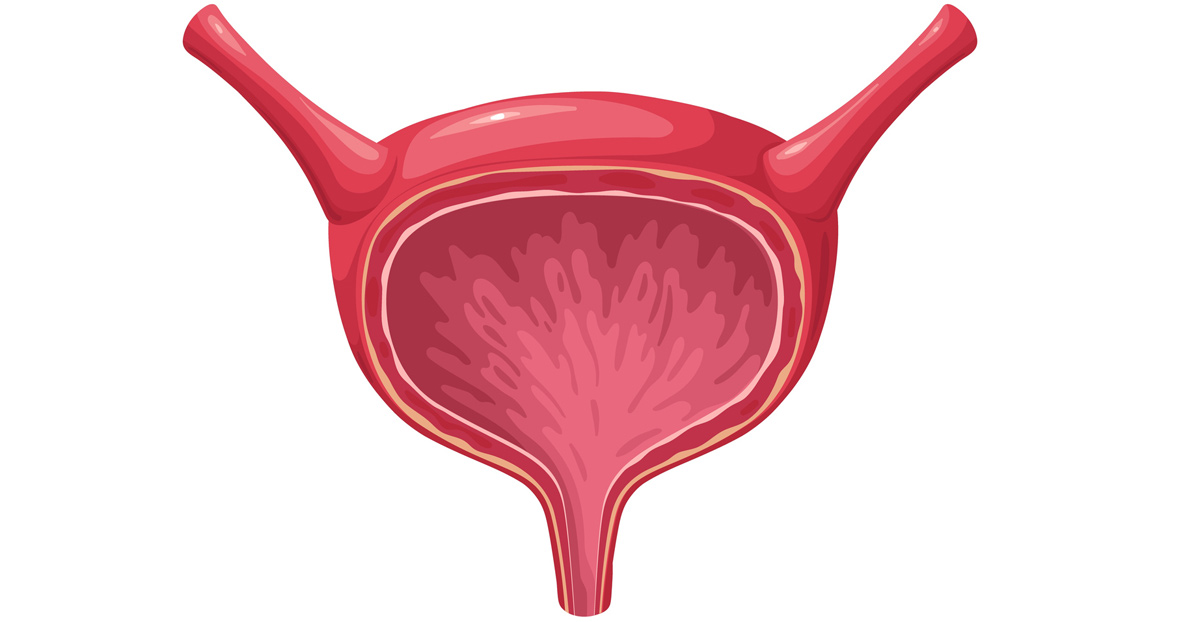
Sacral neuromodulation, also known as sacral nerve stimulation (SNS), is a treatment for various bladder and bowel conditions, such as urinary retention, overactive bladder, urgency urinary incontinence, and anal incontinence.
How Sacral Neuromodulation Works
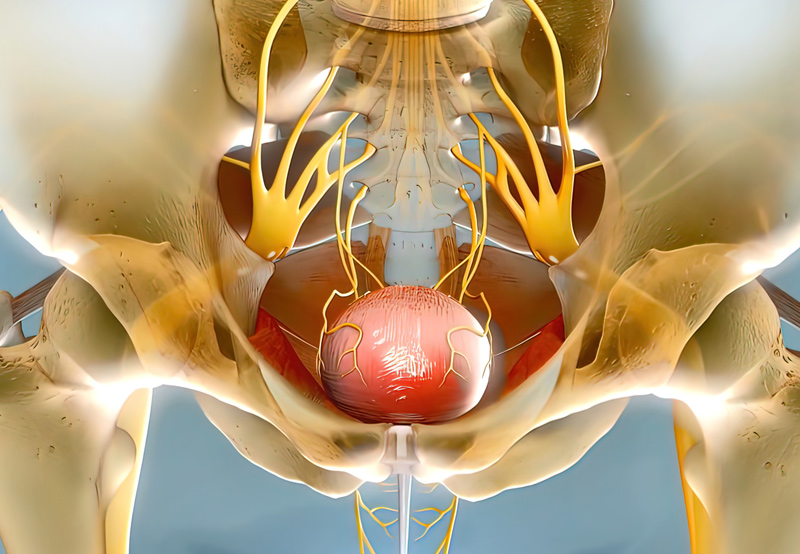
An implantable neurostimulator sends mild electrical signals to a nerve located just above the tailbone to activate or inhibit muscles and nerves that control urinary and bowel function and communicate with the brain.
Treatment alters the function of the sacral nerves and the signals sent to the brain regarding bladder and bowel sensations.
Who Needs Sacral Neuromodulation?
This treatment is for patients who have not benefited from conservative options like medication, lifestyle and dietary changes, and biofeedback.
To determine whether a patient is a good candidate for sacral neuromodulation, the physician may ask them to keep a bladder diary to record toilet habits and symptoms. This information will be used as a base for future comparison.
The Evaluation Phase
A thin temporary wire will be inserted near the sacral nerves in the lower back near the tailbone. The wire will be connected to a small external device that will deliver electrical stimulation to the nerves. The procedure takes less than one hour after which the patient will go home to resume daily activities and record their toilet habits in a new diary for 1 week.
After 1 week of home evaluation, the patient will have a doctor’s appointment to discuss results and assess whether the patient is a good candidate for the treatment. The patient will receive an implanted device depending on the improvements they experienced after the test, quality of life assessments, and patient satisfaction.
The Implant Phase
Patients who are cleared to have the device implanted will undergo a procedure in which the neurostimulator is placed above the buttocks and attached to the implanted wire. The patient will be given a small hand-held controller which will allow them to control the level of stimulation.
The battery’s lifetime can range from five to 10 years. The controller will indicate when the battery is low and needs to be replaced. The wire typically doesn’t need to be replaced or adjusted.
What to Expect During The Procedure
During the test-phase implantation, the patient will receive anesthesia and lay on their stomach. The patient may be asked to describe what they feel during sacral nerve stimulation, whether that is a pulling, tingling, or tapping sensation in their pelvic muscles and vaginal area.
A small wire will be attached to the lead and exit through a small incision in the lower back.
The implant procedure is similar to the initial operation and is typically done one to two weeks later. Once the patient has been given anesthesia, the surgeon will make an incision about two inches long above the buttocks to insert the neurostimulator. The device will be attached to the wire implanted during the first procedure.
Potential Risks of Sacral Neuromodulation
Side effects are rare, but may include infection, pain, and lead movement. These can be resolved with medication, reprogramming of the system, or surgery.
After the procedure, patients are unable to undergo most MRI studies. Patients who need an MRI will need to have their wire and battery removed.
