
Patients diagnosed with pelvic floor dysfunction may need pelvic floor muscle treatment.
Symptoms of Pelvic Floor Dysfunction
Pelvic floor dysfunction occurs when the individual is unable to properly relax and coordinate the muscles in the pelvic floor to urinate or have a bowel movement. Women may also experience pain during sex, while men may struggle with erectile dysfunction.
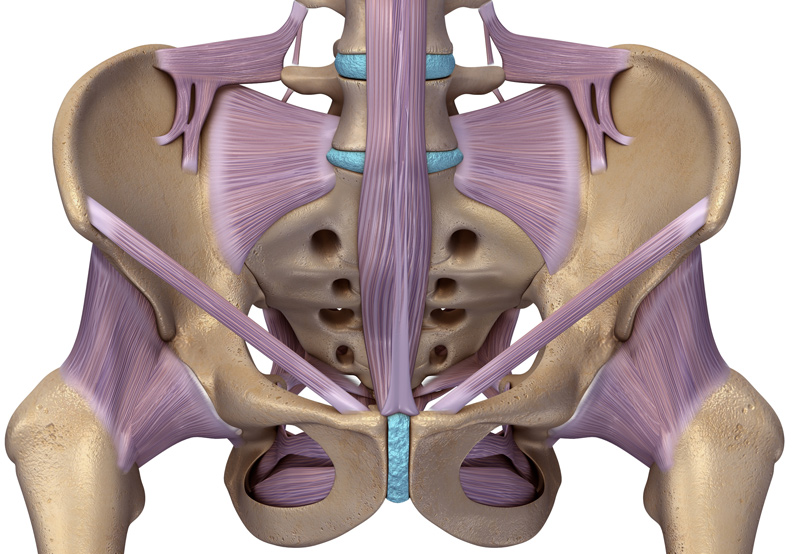
The pelvic organs include the bladder, uterus, vagina, prostate, and rectum. The pelvic floor muscles support these organs by wrapping around the pelvic bone and rectum. Patients with pelvic floor dysfunction may have:
- Difficulty releasing a bowel movement
- An incomplete bowel movement
- Leakage of urine or stool
- Painful urination
- Frequently needing to urinate
- Constipation
- Pain in the lower back
- Ongoing pain in the pelvic region, rectum, or genitals

Causes of Pelvic Floor Dysfunction
Potential causes of the condition include:
- Older age
- Being overweight or obese
- Pregnancy and labor
- Traumatic injury to the pelvic area
- Pelvic surgery
- Overusing the pelvic muscles, leading to poor muscle coordination
Pelvic Floor Dysfunction in Women
Women with pelvic floor dysfunction may also experience:
- Issues with reproductive health affecting the uterus and vagina
- Pelvic organ prolapse
Diagnosing Pelvic Floor Dysfunction
During a doctor’s appointment, the physician may ask the following questions:
- Do you have a history of urinary tract infections?
- Have you been diagnosed with interstitial cystitis or irritable bowel syndrome?
- Do you struggle to pass a bowel movement?
Women will also be asked if they’ve given birth and if they experience pain during sex.
The physician will also do a physical exam to test the patient’s ability to control their pelvic floor muscles, and check for knots, spasms, and weaknesses in these muscles. Some patients may need an intrarectal exam or vaginal exam.
Depending on the results of the physical exam, patients may need to undergo the following tests:
- Anorectal manometry to test pressure, muscle strength, and coordination in the anal sphincters.
- Surface electrodes to test pelvic muscle control.
- Defecating proctogram to show the patient’s ability to pass a bowel movement and identify potential causes of pelvic floor dysfunction.
- Uroflow test to determine the patient’s ability to empty their bladder.
Pelvic Floor Muscle Treatment Options
Non-surgical treatment for pelvic floor dysfunction may include:
- Biofeedback. Special sensors and video will be used to monitor the patient’s pelvic floor muscles as they try to relax or clench them. The physical therapist will then provide feedback and work with the patient to improve muscle coordination.
- Pelvic floor physical therapy. The physical therapist will guide the patient through exercises to strengthen or stretch muscles in the lower back, pelvis, and pelvic floor.
- Medication. Stool softeners can help patients achieve soft and regular bowel movements.
- Relaxation techniques. Medication, yoga, warm baths, acupuncture, and light exercise can help the patient relax.
Injections For High Tone Pelvic Floor Muscles
Patients with hypertonic pelvic floor may be treated with trigger point injections, such as Botox and corticosteroids to alleviate symptoms.
