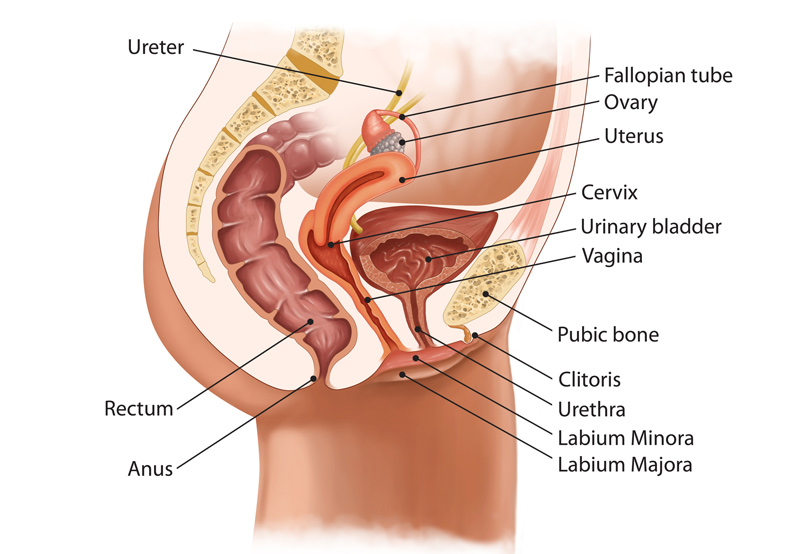

Minimally invasive sacrocolpopexy is done to treat pelvic organ prolapse, a condition caused by a weakening of the pelvic floor. The pelvic organs include the vagina, uterus, bladder, cervix, urethra, intestines, and rectum. These organs are held in place by a group of muscles and tissue. If these muscles and tissue become stretched, weakened, or torn, the pelvic organs may slip out of place or sag, creating prolapse.
Different Types of Prolapse
Depending on organ or organs involved, patients may be diagnosed with one of the following types of pelvic organ prolapse:
- Vaginal vault prolapse. Occurs when the top of the vagina drops down into the vaginal canal.
- Uterine prolapse. Occurs when the uterus and cervix drop down into the vaginal canal.
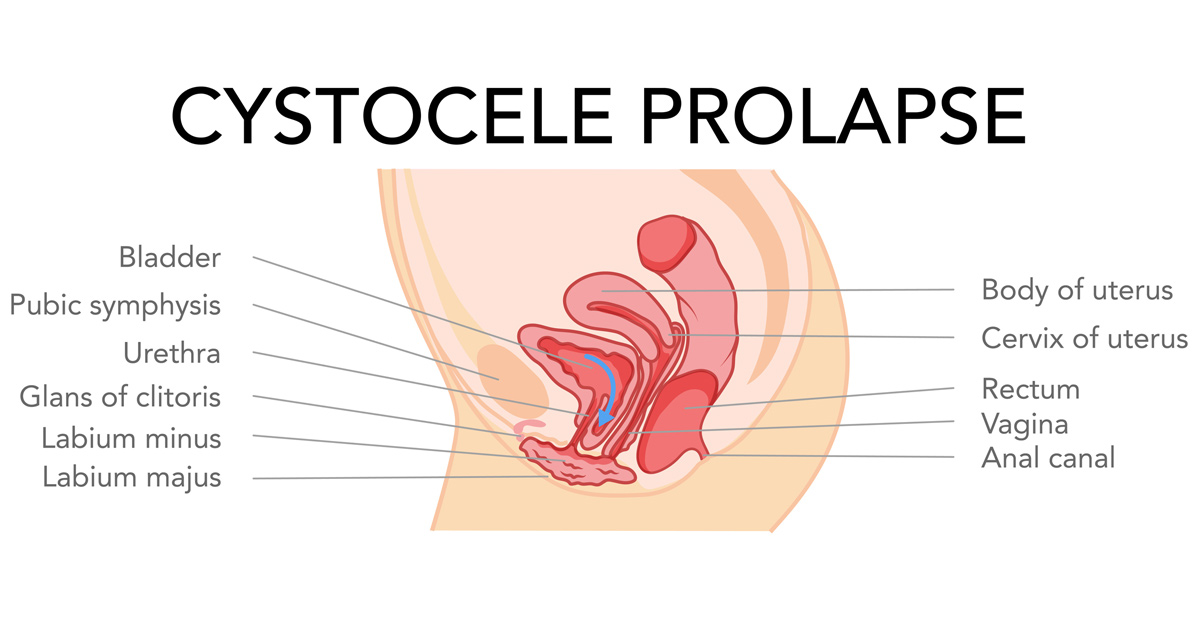
- Cystocele. When the bladder bulges into the vagina.
- Rectocele. When the rectum bulges into the vagina.
- Enterocele. When the small intestine bulges against the vaginal wall.
Repairing Prolapse With Sacrocolpopexy
During sacrocolpopexy, the surgeon attaches surgical mesh from the vagina to the sacrum, which is the tailbone located at the base of the spinal cord.
The procedure is typically performed laparoscopically through the following steps:
1. The patient is placed under general anesthesia.
2. The surgeon makes four to five incisions in the abdomen.
3. Carbon dioxide gas is used to inflate the abdomen and create space for the surgery to be performed.
4. A laparascope and other instruments are inserted through the incisions.
5. The surgeon will attach a piece of surgical mesh to the front and back walls of the vagina and to the sacrum to suspend the top of the vagina or cervix back into the right position.
6. The surgeon will remove the uterus but may leave the cervix intact. Some patients may have their Fallopian tubes and/or ovaries removed.
7. The surgeon may repair the bladder or rectum through the vagina if there isn’t enough support.
8. Patients with urinary incontinence will have a small piece of mesh placed under the urethra to provide support.
9. A small camera will be used to examine inside the bladder to ensure there were no injuries during surgery.
10. The surgeon will remove the instruments and close the incisions with absorbable stitches.
The entire procedure takes two to three hours.
The Recovery Process
Once the patient awakens, staff will do a voiding trial to see if the catheter in the bladder can be removed before hospital discharge. The bladder will be filled with saline and a nurse will remove the catheter. Patients who are able to void ⅔ of the saline will be discharged without a catheter.
If the patient is unable to completely empty the bladder, then the catheter will be replaced and a nurse will teach the patient how to care for it. A repeat voiding trial will be done in three to five days.
Patients will need to keep the incisions clean, dry, and uncovered. It’s important to wash the hands before touching the incisions, changing any dressings, and eating.
After surgery, patients should:
- Drink plenty of fluids
- Eat bland, low-fat foods like Jell-O, chicken broth, and crackers
- Avoid fatty foods to prevent nausea
- Walk around the home to exercise the calf muscles and prevent blood clots
Potential Side Effects And Risks
After surgery, patients may experience gas, pain, abdominal swelling, and shoulder pain for 24 to 72 hours due to the gas that was used to inflate the abdomen. Pain medication may be taken for the first 24 hours to alleviate discomfort.
