
The autologous fascial sling is created from a strip of the patient’s tissue taken from the lower abdomen or thigh to address stress urinary incontinence (SUI) in women. The non-mesh sling supports pelvic floor muscles and helps the urethra withstand increased abdominal pressure transmitted to the bladder.
Symptoms of Stress Urinary Incontinence
Women with stress urinary incontinence may leak urine during any activity that increases abdominal pressure, such as sneezing, laughing, coughing, exercising, standing up, bending over, or lifting something heavy.
Causes of Stress Urinary Incontinence
If the pelvic floor becomes stretched, weakened, or damaged, women may experience SUI. Pregnancy, labor, delivery, chronic coughing, nerve injuries to the lower back, and pelvic surgery can weaken the pelvic muscles.

Risk Factors For SUI
The risk factors of SUI include:
- Smoking
- Pregnancy, labor, and delivery
- Being overweight or obese
- Chronic coughing
- Being female
- Pelvic or prostate surgery
- Nerve injury to the lower back
Who Needs an Autologous Fascial Sling?
Patients may benefit from an autologous fascial sling if they want to avoid synthetic material, if a synthetic midurethral sling cannot be used, and if previous surgery for stress urinary incontinence didn’t alleviate symptoms.
Preparing For Surgery
Prior to surgery, the patient will submit a urine sample that will be tested for signs of a urinary tract infection (UTI). Patients with a UTI will need to take antibiotics before and after the operation.
Before undergoing surgery, patients will receive instructions for preparing for the procedure. If the patient will need general anesthesia, then they should avoid eating, drinking, and smoking for six hours before the procedure. Patients may need to pause taking certain prescription medication a few days before surgery. The physician will offer direction for pausing and resuming medication.
What to Expect During Surgery
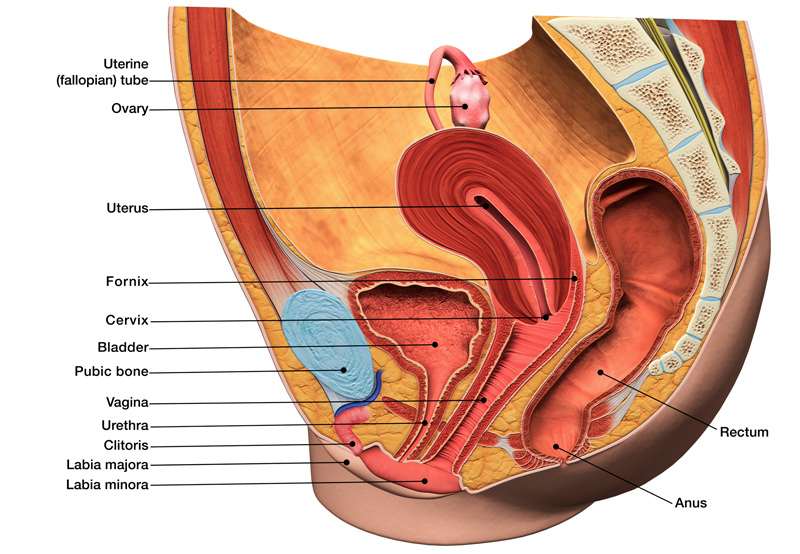
Once the patient has been placed under general anesthesia, the surgeon will:
- Insert a catheter to ensure the bladder is completely empty during surgery.
- Make a horizontal cut a few centimeters long in the lower abdomen and remove a strip of fascia from the rectus muscle.
- Close the fascial and make a small cut in the front of the vaginal wall.
- Place the fascial strip under the urethra near the bladder and attach it just above the public bone.
- Secure the sling with suture material.
- Examine the bladder through a cystoscopy to rule out injury to the organ.
The Recovery Process
Patients will need to stay in the hospital for two to three days after surgery, but may need to stay longer if they’re unable to urinate or if their bladder isn’t emptying completely.
Total recovery time is about six weeks. Patients may have pain in the pelvic area or when they urinate. To support recovery, patients should:
- Drink one to two liters of fluid every day
- Avoid lifting anything heavier than a few pounds
- Avoid heavy exercise
- Take showers instead of baths
- Avoid thermal baths and the sauna
- Eat plenty of fiber to prevent constipation
- Avoid vaginal penetration
Patients should call their doctor and seek immediate medical attention if they develop a fever, are unable to urinate, experience heavy blood loss or pain, have pain in the wound, or if the wound starts to bleed or leak clear fluid.
