
Urinary incontinence treatment may involve lifestyle changes, medical devices, bulking agents, medication, surgery, and electrical nerve stimulation.
Lifestyle Changes
Making changes in daily habits can help improve symptoms across two types of urinary incontinence:
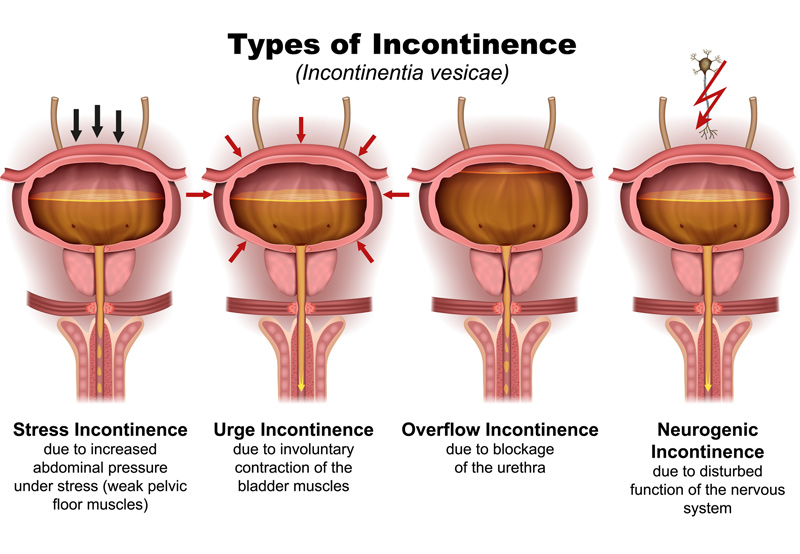
- Stress incontinence. Occurs when movements like sneezing or lifting apply pressure to the bladder.
- Urge incontinence. Occurs when individuals have a sudden, uncontrollable need to urinate.
Patients will keep a bladder diary that they’ll use to record:
- Daily fluid intake
- Activities that led to leakage
- Urination frequency
The patient’s physician will use insights from the bladder diary to create a schedule and help patients go longer between bathroom visits. This will help stretch the bladder and improve symptoms.

Pelvic floor exercises, also known as Kegel exercises, are an effective way to strengthen the pelvic floor. Patients will be taught to tighten and relax their muscles to help control urine flow.
Quitting smoking is critical to improving symptoms of urinary incontinence. Smoking increases coughing, which makes it difficult to hold urine and irritates the muscles in the bladder.
Urgency suppression is another technique used to treat urinary incontinence. Deep breathing, mental distraction, and Kegel exercises can help patients control the sudden need to urinate.
Medical Devices
Urethral inserts and vaginal pessaries can help treat stress incontinence. A urethral insert is a disposable device that can act as a barrier to prevent leakage during certain activities. A vaginal incontinence pessary can help support a prolapsed bladder.
Bulking Agents
Bulking material can be injected in a doctor’s office to plump up tissue around the urethra to make the urethra more narrow to reduce the amount of urinary leakage. Bulking agents are only for patients diagnosed with stress incontinence.
Medication
Medications may reduce bladder spasms.
Surgery
If conservative treatments don’t ease symptoms of urinary incontinence, patients may need to undergo surgery:
- Sling procedure. The surgeon will use mesh and tissue to create a hammock that will support the urethra. Surgery is done with local anesthesia and patients can go home the same day.
- Retropubic colposuspension. The surgeon will make stitches to lift up and support tissues at the entrance of a prolapsed bladder.
Electrical Nerve Stimulation
Urge incontinence may be treated with electrical pulses that stimulate the bladder and change the way it behaves. The two surgical procedures are:
- Sacral nerve stimulation. Once the patient is sedated, the surgeon will implant a stimulator under the patient’s skin in their lower back. The stimulator will send electrical impulses to block messages from the bladder to the bladder signaling the need for urination. These pulses can also increase blood flow to the bladder, strengthen pelvic muscles, and release pain-blocking agents.
- Tibial nerve stimulation. A stimulator will trigger the tibial nerve and send signals to the spine, where it affects the nerves that control the bladder.
