
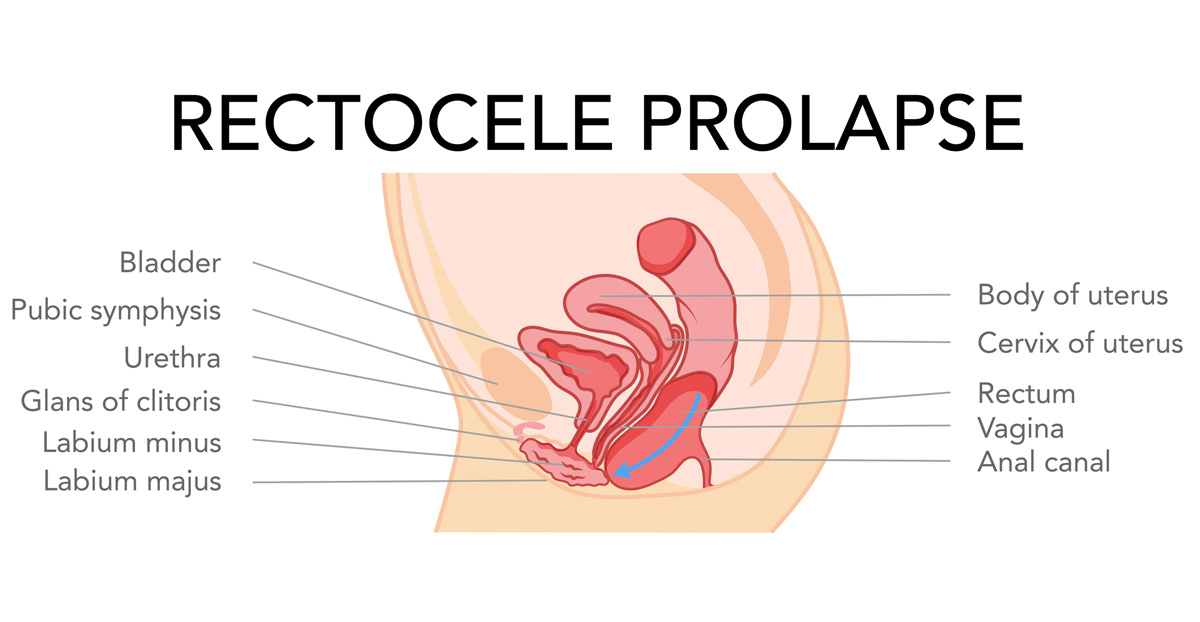
A rectocele is an abnormal bulge in the front wall of the rectum into the back wall of the vagina. The rectum is the bottom part of the colon.
Rectoceles are most common in women over the age of 60, however anyone can get a rectocele.
Symptoms of Rectocele
A small rectocele typically doesn’t cause any symptoms, but a large rectocele can create a noticeable bulge into the vagina and lead to the following symptoms:
- Rectal pain
- Constipation
- Straining with bowel movements
- Fecal impaction in the bulge of the rectum
- Difficulty making a complete bowel movement
- The urge to have multiple bowel movements during the day
- The need to press against the vagina and/or space between the rectum and the vagina to have a bowel movement
- Vaginal bleeding
- Pain with sexual intercourse
- A sense of fullness in the vagina
Causes of Rectocele
Thinning of the rectovaginal septum (which is the tissue between the rectum and vagina) and weakening of the pelvic floor muscles can lead to a rectocele. A few factors that can lead to weakening of the pelvic floor include:
- History of constipation
- Vaginal deliveries
- Chronic straining with bowel movements
- Gynecological or rectal surgeries
- Trauma sustained during vaginal delivery (suc has the use of forceps or vacuum during delivery, tearing, or episiotomy)
- Aging
- Chronic cough or bronchitis
- Repeated heavy lifting
- Obesity
- Prior pelvic surgery, such as a hysterectomy
Diagnosing Rectocele
A rectocele may be discovered during a routine physical examination, but other tests may be necessary to evaluate its severity or association with other symptoms. A pelvic exam will involve checking the vaginal canal for signs of prolapse. The patient may also be asked to squeeze and relax their pelvic floor muscles as if they were stopping a stream or urine. The physician may ask the patient to apply pressure to their gut or strain as if they were defecating to help see the prolapse.
A defecography is a special X-ray test that shows changes in the rectum and anal canal during defecation. This test can pinpoint the size of the rectocele and the degree to which the rectum is emptied.
Treatment Options For Rectocele
Prior to treatment, a physician will determine whether the rectocele is the sole cause of symptoms.
Nonsurgical treatment will focus on promoting good daily bowel habits and avoiding constipation and straining with bowel movements. Preventative and medical steps patients can take include:
- Stool softener
- Eating a high-fiber diet
- Taking over-the-counter fiber supplements
- Drinking at least 6-8 glasses of water per day
- Applying pressure to the back of the vagina during bowel movements
- Doing pelvic floor exercises such as Kegel
- Hormone replacement therapy
- Biofeedback to improve rectal sensation and pelvic floor muscle contraction
Surgical treatment is considered if nonsurgical methods haven’t improved or alleviated symptoms. Abdominal, rectal, or vaginal surgery are a few treatment options for rectocele. The type of procedure that is done will depend on:
- The size of the rectocele and its symptoms
- The patient’s age and general health
- The degree of the prolapse
- The patient’s desire for future pregnancies
- The patient’s desire to continue having sexual intercourse
The goal of treatment is to:
- Remove the extra tissue formed by the rectocele
- Strengthen the wall between the rectum and vagina using surrounding tissue or a mesh patch
The risk of surgery to correct a rectocele include infection, bleeding, pain during intercourse, and recurring or worsening rectocele.
