
Urethral prolapse, also known as urethrocele, is when the urethra protrudes from the urinary opening. The rare but not life-threatening condition typically affects prepubescent girls.
What Happens During Urethral Prolapse
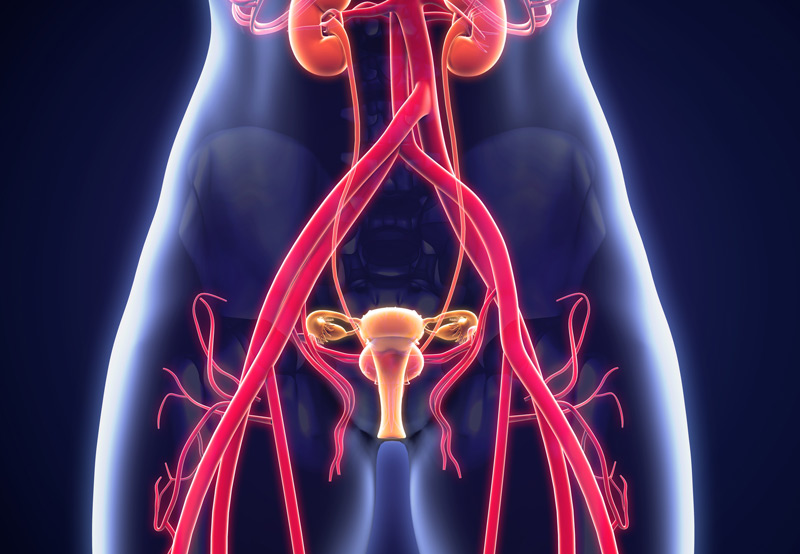
In urethral prolapse, the inner lining of the urethra protrudes from the urinary opening. The tube-shaped urethra carries urine from the bladder and extends from the bladder to the front of the vagina. A protruding urethra looks like an unusually large pink doughnut.
Symptoms of Urethral Prolapse
Most children with urethral prolapse don’t experience any symptoms, but some may have blood spots on their underwear or diaper or tenderness when wiping themselves in the bathroom.
Postmenopausal women with urethral prolapse may experience pain with urination, frequent urination, blood in the urine, and an increased need to urinate at night. In rare cases, urethral prolapse may cause pain with sexual intercourse.

Causes of Urethral Prolapse
The direct cause of urethral prolapse is unknown, but risk factors include:
- Chronic cough
- Constipation
- Genetic predisposition
- Urinary tract infection (UTI)
- Being overweight or obese
- Malnutrition
- Trauma
- Physical exertion
Increased pressure inside the abdomen and weak tissue around the urethra may lead to urethral prolapse. Low levels of estrogen hormone before puberty is associated with the condition.
The condition may also occur when tissues around the urethra are weak or when the muscles fail to properly connect to the urethral skin. Prepubescent African American girls aged five to eight years old are most likely to have urethral prolapse.
The risk of urethral prolapse is higher in women who have been pregnant and given birth. Pressure and strain on the abdominal and pelvic region can damage the pelvic floor muscles and the tissues that support the urethra.
Diagnosing And Treating Urethral Prolapse
The condition is typically found during a routine physical examination. In adult patients, a cystourethroscopy may also be done to confirm diagnosis.
Girls who don’t have any symptoms may not need treatment. But patients who are exhibiting symptoms may benefit from the following treatments:
1.Estrogen cream. A hormone cream can be applied for a short period of time (two to three times a day for two weeks) to help strengthen the tissues supporting the urethra and resolve mild symptoms. But children receiving estrogen treatment should be monitored for known side effects such as breast budding, pubic hair, and general irritation.
2.Lifestyle changes. Overweight or obese women should consider losing weight and avoiding heavy lifting to reduce the risk of recurrence.
3.Treating constipation. Children with constipation should be treated to prevent straining during bowel movements. This will help heal prolapsed tissue.
4.Vaseline. Vaseline, a petroleum jelly, can help alleviate sensitivity or tenderness by acting as a barrier.
5.Sitz baths. Short, 15- to 20-minute baths taken twice a day can help heal the urethral prolapse and keep the area clean
6.Surgery. If conservative treatments fail to alleviate symptoms, patients may need to undergo surgery to cut away the protruding tissue and sew the lining back together. Catheterization will be necessary for a brief period of time after surgery.
